Advancements in medical education: emerging aspects and innovations

UDC 613:002.8.:378:616-052+378
DOI : https://doi.org/10.61948/prevmed-2024-2-25
S. S. Boieva1, O. A. Raksha-Sliusareva2, A. Sliusarev2, Р. G.Kovalenko2
1. Lithuanian University of Helth Sciences, Kaunas, Lithuania
2. Donetsk National Medical University, Lyman, Ukraine
The landscape of medical education is indeed in a state of profound transformation, spurred by emerging aspects and innovative approaches that are responsive to the ever-evolving demands of the healthcare sector.
This comprehensive review delves into the contemporary trends within medical education, emphasizing the integration of various elements such as technology, interprofessional education, personalized learning, telemedicine, ethics and professionalism education, global health education, and wellness and resilience initiatives.
These advancements serve a multifaceted purpose, aiming to enrich both the teaching and learning experience within medical education. By leveraging technology, educators can provide immersive learning opportunities that transcend traditional boundaries. Interprofessional education stands as a cornerstone in fostering collaborative practices among healthcare professionals, instilling a comprehensive approach to patient care that is inclusive of diverse perspectives and expertise. Moreover, personalized learning methodologies cater to the unique needs of individual learners, ensuring a more tailored and effective educational experience. Telemedicine platforms further expand access to educational resources and experiences, overcoming geographical barriers and promoting inclusivity within medical education. Ethics and professionalism education emerge as vital components in shaping the moral compass of future healthcare professionals, guiding them toward ethical decision-making and upholding the highest standards of professionalism. Global health education equips students with the necessary skills and knowledge to navigate the complexities of healthcare on a global scale, preparing them to address international healthcare challenges with competence and compassion. Additionally, wellness and resilience initiatives take center stage in safeguarding the mental and physical well-being of medical students and practitioners alike. By prioritizing the holistic health of healthcare professionals, these initiatives contribute to the cultivation of resilient individuals who are better equipped to thrive in the demanding landscape of healthcare.
Key words: Medical education, technology integration, interprofessional education, personalized learning, telemedicine, ethics, professionalism, global health, wellness, resilience.
УСПІХ МЕДИЧНОЇ ОСВІТИ:НОВІ АСПЕКТИ ТА ІННОВАЦІЇ
С. С. Боєва1, О. А. Ракша-Слюсарева2, О. А. Слюсарев2, П. Г. Коваленко2
1. Литовський університет наук про здоров’я, Каунас, Литва
2. Донецький національний медичний університет, Лиман, Україна
Ландшафт медичної освіти справді перебуває в стані глибокої трансформації, що стимулюється новими аспектами та інноваційними підходами, які реагують на постійно змінювані вимоги сектору охорони здоров’я. У цьому всебічному огляді розглядаються сучасні тенденції в медичній освіті, наголошується на інтеграції різних елементів, таких як технології, міжпрофесійна освіта, персоналізоване навчання, телемедицина, освіта етики та професіоналізму, глобальна медична освіта, а також ініціативи з оздоровлення та стійкості.
Ці досягнення служать багатогранній меті, спрямованій на збагачення як викладання, так і досвіду навчання у медичній освіті. Використовуючи технологію, викладачі можуть надати захоплюючі можливості навчання, які виходять за межі традиційних рамок. Міжпрофесійна освіта є наріжним каменем у сприянні співпраці між медичними працівниками, прищеплюючи комплексний підхід до догляду за пацієнтами, який включає різноманітні погляди та досвід. Крім того, персоналізовані методики навчання задовольняють унікальні потреби окремих учнів, забезпечуючи більш адаптований та ефективний навчальний досвід. Телемедичні платформи ще більше розширюють доступ до освітніх ресурсів і досвіду, долаючи географічні бар’єри та сприяючи інклюзивності в медичній освіті. Освіта етики та професіоналізму є життєво важливими компонентами у формуванні морального компасу майбутніх медичних працівників, спрямовуючи їх до прийняття етичних рішень та дотримання найвищих стандартів професіоналізму. Глобальна медико-санітарна освіта дає студентам необхідні навички та знання, щоб орієнтуватися в складних деталях охорони здоров’я в глобальному масштабі, готуючи їх до вирішення міжнародних викликів охорони здоров’я з компетентністю та співчуттям. Водночас ініціативи щодо оздоровлення та стійкості посідають центральне місце у захисті психічного та фізичного благополуччя як студентів-медиків, так і практикуючих лікарів. Віддаючи пріоритет цілісному здоров’ю медичних працівників, ці ініціативи сприяють вихованню стійких людей, які краще підготовані для процвітання у складних умовах охорони здоров’я.
Ключові слова: медична освіта, інтеграція технологій, міжпрофесійна освіта, персоналізоване навчання, телемедицина, етика, професіоналізм, глобальне здоров’я, здоров’я, стійкість.
In response to the projected global demand for healthcare services and the anticipated creation of 40 million new jobs in the healthcare sector by 2030 [1], medical education is undergoing a significant transformation. One pivotal change, as visualized in the accompanying (Figure1), is the integration of advanced technology into the curriculum.
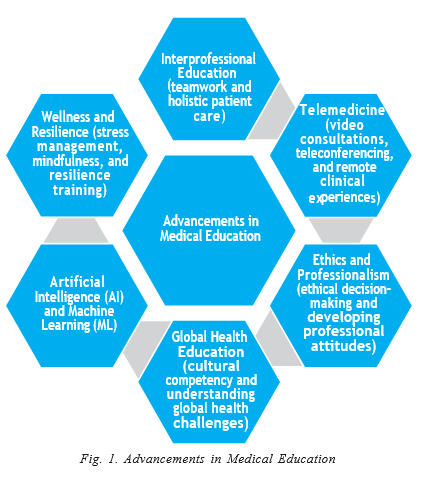
This modern approach, moving beyond the traditional, high-cost hospital-based model [2] embraces innovative tools like virtual reality (VR) and augmented reality (AR). VR technology, as described by Haowen et al. [3], provides medical students with the opportunity to practice in controlled, realistic environments, thereby enhancing their practical skills and decision-making capabilities. Similarly, AR technology, as explored by Dhar et al. [4], superimposes digital information onto real-world scenarios, enriching the learning experience with interactive simulations of complex medical concepts [2].
Additionally, the use of simulation software [5], online learning platforms, and mobile applications is revolutionizing the way medical education is delivered. These advancements afford students access to a more extensive range of educational resources and the flexibility to learn at their own pace, thereby fostering a more personalized and adaptive learning experience.
To further elucidate the impact of these emerging aspects and innovations, a comparative analysis was conducted, contrasting the traditional and contemporary paradigms in medical education. The findings of this analysis are summarized in Table 1, providing a clear juxtaposition of the divergent teaching methods, learning outcomes, and levels of student engagement characteristic of each approach.
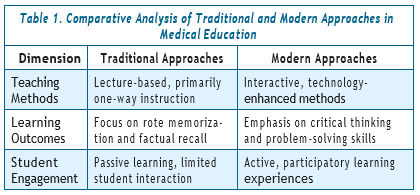
This table underscores a shift from passive reception in traditional settings to an active, engaging, and technology-imbued learning environment in the modern medical educational landscape. These innovations address the current shortfall of healthcare workers and provide the foundation for cultivating future professionals equipped with vital skills for success in an ever-evolving healthcare context.
Moreover, the integration of digital tools has markedly improved access to educational resources in the field. Online platforms now offer an extensive range of interactive textbooks, medical journals, multimedia lectures, and educational videos. This plethora of resources is readily accessible, facilitating self-directed learning and allowing students to review content at their preferred pace, thereby fostering a more personalized and flexible learning approach [6]. Additionally, technology plays a pivotal role in enhancing collaborative learning and effective communication among students and educators. The use of online discussion forums, virtual classrooms, and video conferencing platforms not only enables active participation in group discussions but also promotes the sharing of knowledge and clarification of concepts among peers and instructors. These digital tools are instrumental in developing essential skills such as teamwork, critical thinking, and the ability to exchange diverse perspectives, thus significantly enhancing the overall medical educational experience [7].
The integration of digital tools and adaptive learning platforms in medical education is a transformative development, enabling personalized learning experiences tailored to the specific needs of individual students. These innovative platforms use algorithms to evaluate student performance, providing customized feedback and learning materials. This approach to personalized learning supports self-paced study, effectively addresses individual learning deficiencies, and ultimately enhances overall educational outcomes. By adapting to the unique needs and learning styles of each student, digital technologies offer a more tailored and efficient educational experience [8]. Furthermore, the incorporation of technology in medical education plays a crucial role in supporting the professional development and lifelong learning of healthcare professionals. A range of online resources, including webinars and virtual conferences, provide convenient avenues for professionals to stay updated with the latest research, medical advancements, and evidence-based practices. This focus on continuous learning and professional growth cultivates a culture of continuous improvement and ensures the provision of high-quality healthcare services. Digital technologies, by offering accessible and current educational opportunities, contribute significantly to the ongoing development and refinement of healthcare professionals’ knowledge and skills throughout their careers [9].
While the integration of technology in medical education presents numerous benefits, it is essential to recognize and address the potential challenges and limitations of this approach. These challenges include ensuring the availability of adequate infrastructure, providing necessary training for faculty and students, safeguarding data privacy and security, and maintaining a balance between the use of technology and the development of interpersonal skills.
Despite these challenges, the integration of technology into medical education introduces new and dynamic dimensions that are in line with the evolving trends and advancements within the discipline. This review underscores several significant emerging aspects of education in medical universities, reflecting the changing landscape of the field.
Interprofessional Education (IPE) represents an innovative educational approach, recognizing the critical importance of collaborative efforts among healthcare professionals from varied disciplines. Medical universities are increasingly incorporating IPE into their curricula, aiming to foster teamwork, effective communication, and comprehensive patient care. IPE programs unite students from diverse fields such as medicine, nursing, pharmacy, dentistry, and allied health professions, with a core goal of developing a mutual understanding of the roles, responsibilities, and expertise of each profession. This approach promotes a holistic patient care methodology. In practice, IPE initiatives include interactive learning activities like case-based discussions, team-based projects, and simulated patient scenarios, alongside interprofessional clinical experiences. These activities are designed to encourage collaboration and knowledge exchange among students, enabling them to address complex healthcare challenges effectively. A notable case study from a medical university revealed that implementing IPE activities, particularly team-based projects and clinical experiences, significantly improved collaboration and communication skills among students from various healthcare disciplines. This study reported advancements in teamwork capabilities, a deeper understanding of professional roles, and a more integrated approach to patient care [10].
The advantages of IPE are manifold, encompassing improved communication skills, enhanced teamwork and collaboration, holistic patient care, increased respect and understanding among healthcare professionals, and opportunities for professional networking. Notably, IPE aids in developing effective communication skills, essential for seamless collaboration within interprofessional healthcare teams. By interacting with peers from different healthcare disciplines, students enhance their ability to communicate ideas clearly, concisely, and respectfully. Additionally, IPE fosters a strong sense of teamwork and collaboration among future healthcare professionals, encouraging them to value and understand the unique contributions of each discipline. This leads to a more inclusive and effective healthcare team dynamic. Holistic patient care is another critical benefit of IPE. By incorporating diverse perspectives and disciplines, IPE ensures a comprehensive approach to patient care, resulting in superior patient outcomes and improved healthcare service delivery [11]. Moreover, IPE enhances mutual respect and understanding among students for various healthcare professions, breaking down professional barriers and fostering an inclusive healthcare environment. Finally, IPE offers significant networking opportunities, allowing students to form professional relationships and networks vital for their future careers. These connections promote interprofessional collaboration and knowledge sharing, essential for continuous professional growth and development [12]. In summary, the benefits of IPE, such as enhanced communication, teamwork, holistic care, respect for diverse healthcare professions, and networking opportunities, are instrumental in nurturing competent and collaborative healthcare professionals, thereby elevating the overall quality of patient care and healthcare outcomes.
Telemedicine and remote learning have emerged as indispensable tools in modern medical education, offering students unparalleled opportunities for remote engagement in patient care. Through telemedicine technologies, students can actively participate in virtual consultations, observe a wide range of medical procedures and surgeries, and remotely access patient records, thereby enriching their clinical knowledge and honing their decision-making skills [13].
Medical universities are increasingly recognizing the potential of telemedicine tools such as teleconferencing, video consultations, remote clinical experiences, and virtual simulations to expand educational horizons beyond the confines of traditional classroom settings. Recent research underscores the value of these approaches, demonstrating that students derive significant benefits from virtual classrooms and video consultations by gaining insights into various clinical scenarios and enhancing their understanding of different medical specialties [14].
Telemedicine, leveraging advanced technology, facilitates virtual healthcare interactions, enabling universities to extend educational resources to diverse geographical locations. Teleconferencing platforms enable students to engage in interactive sessions from virtually anywhere, thereby enhancing flexibility and accessibility. Similarly, video consultations provide students with hands-on learning experiences, allowing them to observe and interact with patients remotely, thereby refining essential clinical skills such as history-taking, physical examination, and patient communication.
Moreover, remote clinical experiences immerse students in a variety of clinical settings, broadening their understanding of medical specialties and providing valuable exposure to real-world healthcare practices. This includes the opportunity for students to conduct physical examinations remotely, under the guidance of healthcare professionals, ensuring they develop proficiency in this essential aspect of patient care.
While telemedicine and remote learning offer significant advantages, their successful implementation poses challenges that must be addressed. These challenges include the need for robust technological infrastructure, concerns regarding patient privacy and data security, and limitations in practical skills training. To effectively integrate telemedicine into medical education, universities must develop comprehensive strategies and provide adequate support to address these challenges [15].
In conclusion, telemedicine has revolutionized medical education, offering students unparalleled opportunities for remote learning and engagement, including hands-on experiences such as physical examination. By harnessing telemedicine tools effectively, medical universities can transcend physical boundaries, provide students with comprehensive educational experiences, and better prepare the next generation of healthcare professionals to meet the challenges of modern healthcare delivery. However, careful planning, continuous evaluation, and ongoing support are essential to overcome challenges and ensure the successful integration of telemedicine into medical education.
Artificial Intelligence (AI) and Machine Learning (ML) are increasingly being recognized for their substantial contributions to medical education. As medical universities explore the integration of these technologies, they uncover promising opportunities to enhance the learning experience. AI and ML are particularly influential in aspects such as diagnostic reasoning, personalized learning pathways, and predictive analytics, leading to more precise and effective healthcare practices [16].
AI and ML excel in supporting diagnostic reasoning by analyzing extensive medical data, including images, patient records, and clinical guidelines. Their capacity for pattern recognition and data analysis enables them to aid in identifying potential diagnoses, emphasizing important features in medical images, and providing evidence-based recommendations for clinical decision-making. This augmentation of the diagnostic process is pivotal in enhancing both accuracy and efficiency within medical education.
Personalized learning pathways represent another significant impact area for AI and ML. By analyzing data specific to individual students, such as performance metrics, learning styles, and preferences, these technologies can customize educational content and recommendations. This tailoring process allows AI and ML algorithms to adjust learning materials, pacing, and assessment methods in a way that optimizes the learning experience, thereby boosting student engagement and knowledge retention [17].
Predictive analytics powered by AI and ML also play a crucial role in medical education. By examining various data sources, including student performance, educational resources, and clinical outcomes, they provide valuable insights into potential improvements in educational strategies and patient care.
Despite these advantages, the integration of AI and ML in medical education comes with challenges. Ethical considerations, data privacy, and algorithm transparency are paramount to ensure the responsible and unbiased use of these technologies. Moreover, both faculty and students may need training and support to effectively use and interpret AI and ML systems’ outputs [18].
In summary, the exploration of AI and ML technologies in medical education offers immense potential. By aiding diagnostic reasoning, facilitating personalized learning, and providing predictive analytics, these technologies have the capacity to significantly transform medical education, contributing to more accurate and effective healthcare practices.
Ethics and professionalism education has increasingly become a focal point in medical universities, underscoring its critical role in healthcare. In response to the growing recognition of the importance of ethical considerations and professionalism, medical universities are actively integrating these subjects into their curricula. These educational initiatives are designed to enhance ethical decision-making, foster empathy, and instill a strong sense of professionalism in future healthcare professionals. The curriculum in ethics education is structured to provide students with the necessary knowledge and skills to effectively navigate the complex ethical dilemmas encountered in healthcare practice. This includes establishing a solid foundation in ethical principles, values, and frameworks that are essential in guiding patient care decisions. Interactive methods such as case-based discussions, role-play-ing exercises, and reflective practices are employed to engage students in critical thinking and ethical reasoning. These techniques aim to strengthen students’ abilities to make principled and informed decisions in challenging healthcare scenarios [19].
In parallel, professionalism education focuses on cultivating the attitudes, behaviors, and values integral to effective and compassionate healthcare practice. This aspect of education addresses core attributes including integrity, accountability, respect, empathy, and cultural competence. To promote these qualities, medical universities implement various strategies like mentorship programs, workshops on professionalism, and reflective activities that encourage self-assessment and self-reflection. These educational approaches are geared toward developing a comprehensive understanding of professionalism and its application in healthcare settings [20].
Global health education is receiving increasing attention in medical universities, reflecting the growing interconnectedness of healthcare systems worldwide. Recognizing the importance of this field, medical universities are focusing on equipping students with the knowledge and skills necessary to meet global health challenges, develop cultural competency, and excel in diverse healthcare environments [21, 22]. The scope of global health education is extensive, covering a wide array of topics such as disparities in global health, infectious and non-communicable diseases, health systems and policies, social determinants of health, and healthcare ethics. Through comprehensive coursework, experiential learning, and field experiences, students are exposed to the complexities and real-world challenges of global health. This educational approach enables students to gain an in-depth understanding of the challenges faced by underserved populations and settings with limited resources. They learn to critically assess the influence of various social, economic, political, and environmental factors on health outcomes on a global scale. This understanding is crucial for students to critically evaluate health systems, pinpoint areas needing improvement, and contribute effectively to initiatives aimed at reducing health disparities.
A crucial aspect of global health education is the development of cultural competency. Students are taught to respect and value diverse cultural beliefs, practices, and values, fostering skills in cross-cultural communication, adaptability, and understanding. This aspect of education is paramount in preparing students to work effectively in diverse healthcare settings. Cultural competency significantly enhances healthcare delivery by ensuring that healthcare providers can effectively interact with patients from varied cultural backgrounds and comprehend the impact of culture on health beliefs and behaviors [23, 24].
The growing recognition of the challenges and stresses inherent in healthcare professions has led to an increased emphasis on wellness and resilience within medical education. Medical universities are now more focused than ever on promoting these aspects to ensure the well-being of their students and their ability to thrive in their future careers.
Wellness initiatives within medical education are designed to support students in maintaining their physical, mental, and emotional health. These programs often encompass a variety of activities, including stress management workshops, mindfulness training, physical fitness regimens, counseling services, and peer support networks. By directly addressing the unique stressors and demands associated with the medical profession, these wellness initiatives strive to prevent burnout, improve overall well-being, and foster a healthy work-life balance for medical students.
In addition to wellness programs, resilience training plays a crucial role in preparing medical students for the challenges they will face throughout their careers. This training emphasizes the development of emotional intelligence, self-awareness, effective communication skills, and strategies for managing stress and adversity. Such training is essential in equipping students to effectively navigate the demanding nature of the medical field, ensuring their personal well-being, and enabling them to provide the highest quality of care to their patients [25].
Discussion
The discussion regarding advancements in medical education sheds light on several pivotal emerging aspects and innovations that are profoundly shaping the field. Notably, the integration of technology has catalyzed a significant paradigm shift in the learning experience. This transformation encompasses a multifaceted approach, encompassing immersive opportunities through virtual reality, the extensive use of online platforms, and collaborative tools. These technological interventions have effectively disrupted traditional teaching methodologies, enabling students to immerse themselves in controlled yet realistic environments. Through VR simulations, students can acquire practical skills and hone their decision-making abilities in a secure and conducive setting. Simultaneously, the integration of online platforms and collaborative tools provides students access to a vast repository of educational resources, thus fostering self-directed learning and adaptability.
Furthermore, the incorporation of interprofessional education stands out as a cornerstone of modern medical education. The essence of IPE lies in fostering a collaborative and cohesive approach to patient care. By bringing together students from diverse healthcare disciplines, this approach imparts invaluable lessons in teamwork, effective communication, and the significance of a holistic approach to patient care. Students gain a profound appreciation for the distinct contributions of each healthcare profession, laying the foundation for seamless collaboration within multidisciplinary healthcare teams. This collaborative spirit ultimately translates into improved patient outcomes and healthcare service delivery.
In tandem with IPE, the concept of personalized learning has garnered substantial attention and recognition within medical education. This innovative approach is facilitated by adaptive learning platforms, which possess the capability to customize educational content to cater to individual student needs. Personalized learning not only enhances student engagement but also promotes self-directed learning, allowing students to take charge of their educational journey. The adaptability of these platforms, in terms of pacing and content delivery, optimizes the learning experience, leading to improved learning outcomes.
Moreover, the advent of telemedicine has significantly expanded the horizons of remote learning in medical education. Leveraging teleconferencing, video consultations, and remote clinical experiences, students are provided with the opportunity to engage in virtual classrooms and gain exposure to diverse healthcare settings. This flexibility and accessibility break down geographical barriers and augment educational access. Consequently, students are exposed to a broader spectrum of clinical scenarios, thus enriching their understanding of various medical specialties and enhancing their clinical decision-making skills. Ethics and professionalism education has rightfully claimed its place in medical curricula. The emphasis on ethical considerations and professionalism equips students with the necessary knowledge and skills to navigate the intricate web of ethical dilemmas often encountered in healthcare practice. Case-based discussions and reflective practices emerge as effective tools in nurturing critical thinking skills and establishing a robust ethical foundation for future healthcare professionals.
Furthermore, global health education plays a pivotal role in preparing students for the challenges posed by an interconnected world. This facet of education imparts an understanding of global health issues, disparities, and cultural competency. It empowers students to work effectively in diverse healthcare enviapproach enables students to gain an in-depth understanding of the challenges faced by underserved populations and settings with limited resources. They learn to critically assess the influence of various social, economic, political, and environmental factors on health outcomes on a global scale. This understanding is crucial for students to critically evaluate health systems, pinpoint areas needing improvement, and contribute effectively to initiatives aimed at reducing health disparities.
A crucial aspect of global health education is the development of cultural competency. Students are taught to respect and value diverse cultural beliefs, practices, and values, fostering skills in cross-cultural communication, adaptability, and understanding. This aspect of education is paramount in preparing students to work effectively in diverse healthcare settings. Cultural competency significantly enhances healthcare delivery by ensuring that healthcare providers can effectively interact with patients from varied cultural backgrounds and comprehend the impact of culture on health beliefs and behaviors [23, 24].
The growing recognition of the challenges and stresses inherent in healthcare professions has led to an increased emphasis on wellness and resilience within medical education. Medical universities are now more focused than ever on promoting these aspects to ensure the well-being of their students and their ability to thrive in their future careers.
Wellness initiatives within medical education are designed to support students in maintaining their physical, mental, and emotional health. These programs often encompass a variety of activities, including stress management workshops, mindfulness training, physical fitness regimens, counseling services, and peer support networks. By directly addressing the unique stressors and demands associated with the medical profession, these wellness initiatives strive to prevent burnout, improve overall well-being, and foster a healthy work-life balance for medical students.
In addition to wellness programs, resilience training plays a crucial role in preparing medical students for the challenges they will face throughout their careers. This training emphasizes the development of emotional intelligence, self-awareness, effective communication skills, and strategies for managing stress and adversity. Such training is essential in equipping students to effectively navigate the demanding nature of the medical field, ensuring their personal well-being, and enabling them to provide the highest quality of care to their patients [25].
Discussion
The discussion regarding advancements in medical education sheds light on several pivotal emerging aspects and innovations that are profoundly shaping the field. Notably, the integration of technology has catalyzed a significant paradigm shift in the learning experience. This transformation encompasses a multifaceted approach, encompassing immersive opportunities through virtual reality, the extensive use of online platforms, and collaborative tools. These technological interventions have effectively disrupted traditional teaching methodologies, enabling students to immerse themselves in controlled yet realistic environments. Through VR simulations, students can acquire practical skills and hone their decision-making abilities in a secure and conducive setting. Simultaneously, the integration of online platforms and collaborative tools provides students access to a vast repository of educational resources, thus fostering self-directed learning and adaptability.
Furthermore, the incorporation of interprofessional education stands out as a cornerstone of modern medical education. The essence of IPE lies in fostering a collaborative and cohesive approach to patient care. By bringing together students from diverse healthcare disciplines, this approach imparts invaluable lessons in teamwork, effective communication, and the significance of a holistic approach to patient care. Students gain a profound appreciation for the distinct contributions of each healthcare profession, laying the foundation for seamless collaboration within multidisciplinary healthcare teams. This collaborative spirit ultimately translates into improved patient outcomes and healthcare service delivery.
In tandem with IPE, the concept of personalized learning has garnered substantial attention and recognition within medical education. This innovative approach is facilitated by adaptive learning platforms, which possess the capability to customize educational content to cater to individual student needs. Personalized learning not only enhances student engagement but also promotes self-directed learning, allowing students to take charge of their educational journey. The adaptability of these platforms, in terms of pacing and content delivery, optimizes the learning experience, leading to improved learning outcomes.
Moreover, the advent of telemedicine has significantly expanded the horizons of remote learning in medical education. Leveraging teleconferencing, video consultations, and remote clinical experiences, students are provided with the opportunity to engage in virtual classrooms and gain exposure to diverse healthcare settings. This flexibility and accessibility break down geographical barriers and augment educational access. Consequently, students are exposed to a broader spectrum of clinical scenarios, thus enriching their understanding of various medical specialties and enhancing their clinical decision-making skills. Ethics and professionalism education has rightfully claimed its place in medical curricula. The emphasis on ethical considerations and professionalism equips students with the necessary knowledge and skills to navigate the intricate web of ethical dilemmas often encountered in healthcare practice. Case-based discussions and reflective practices emerge as effective tools in nurturing critical thinking skills and establishing a robust ethical foundation for future healthcare professionals.
Furthermore, global health education plays a pivot- al role in preparing students for the challenges posed by an interconnected world. This facet of education imparts an understanding of global health issues, dis- parities, and cultural competency. It empowers stu- dents to work effectively in diverse healthcare environments, to critically evaluate health systems, and to advocate for health equity on a global scale. Through comprehensive coursework, experiential learning, and field experiences, students are exposed to the complexities and real-world challenges of global health. This understanding is indispensable for fostering a more profound appreciation of the influence of various social, economic, political, and environmental factors on health outcomes worldwide.
Lastly, the recognition of the demands and stresses intrinsic to healthcare professions has spurred a renewed emphasis on wellness and resilience within medical education. Wellness programs encompass a spectrum of activities aimed at supporting students in maintaining their physical, mental, and emotional health. These initiatives address the unique stressors and demands associated with the medical profession, with a primary goal of preventing burnout and nurturing overall well-being. In parallel, resilience training has become an integral component of medical education, equipping students with emotional intelligence, self-awareness, effective communication skills, and strategies for managing stress and adversity. This training is pivotal in preparing students to navigate the demanding nature of the medical field, ensuring their personal well-being, and enabling them to provide the highest quality of care to their patients.
In conclusion, the contemporary landscape of medical education is undergoing a profound transformation driven by technological integration, collaborative learning, personalized approaches, and an increased focus on ethics, global health, wellness, and resilience. These innovations not only address the current challenges in healthcare workforce availability but also empower future healthcare professionals with the skills and competencies needed to excel in a dynamically evolving healthcare landscape. Nevertheless, it is crucial to recognize and address the challenges and ethical considerations that accompany these advancements to ensure their responsible and effective integration into medical education.
Conclusion.
In summary, this article has explored the dynamic landscape of medical education, shedding light on the innovative approaches and emerging facets that are shaping the future of healthcare training. The integration of technology, interprofessional education, personalized learning, telemedicine, ethics and professionalism education, global health education, and a heightened focus on wellness and resilience collectively represent the forefront of advancements in medical pedagogy.
These developments signify a paradigm shift in how medical knowledge is imparted and absorbed. Technology’s role in creating immersive learning environments is pivotal, while interprofessional education fosters collaboration and emphasizes the importance of holistic patient care. Personalized learning ensures that education aligns with individual student needs, and telemedicine widens the horizons of educational access. Ethics and professionalism education empower students to navigate complex ethical dilemmas, and global health education equips them to address healthcare challenges on a global scale. The prioritization of wellness and resilience reflects a commitment to the well-being of both current and future healthcare professionals.
Incorporating these progressive elements into medical education is no longer a choice but a fundamental requirement. It is essential for nurturing a cohort of healthcare professionals who not only possess the necessary knowledge and skills but also demonstrate empathy, adaptability, and a deep understanding of the diverse healthcare landscape. By embracing these transformative approaches, medical education institutions are poised to not only meet but also exceed the evolving demands of the healthcare field. This, in turn, holds the promise of enhancing healthcare outcomes and improving the overall quality of patient care.
References
- Boniol M., Kunjumen T., Nair T. S., Siyam A., Campbell J., Diallo K. The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Glob Health [Internet]. 2022;7(6):e009316. Available from: http:// doi.org/10.1136/bmjgh-2022-009316
- Van Way CW Thoughts on medical education. Mo Med. 2017;114(6):417–8.
- Haowen J., Vimalesvaran S., Myint Kyaw B., Tudor Car L. Virtual reality in medical students’ education: a scoping review protocol. BMJ Open [Internet]. 2021;11(5):e046986. Available from: http:// doi.org/10.1136/bmjopen-2020-04698
- Dhar P., Rocks T., Samarasinghe R. M., Stephenson G., Smith C. Augmented reality in medical education: students’ experiences and learning outcomes. Med Educ Online [Internet]. 2021;26(1). Available from: http://dx.doi.org/10.1080/10872981.2021.1953953
- Al-Elq Simulation-based medical teaching and learning. J Family Community Med [Internet]. 2010;17(1):35. Available from: http://dx.doi.org/10.4103/1319-1683.68787
- Park J. C., Kwon H. J. E., Chung C. W. Innovative digital tools for new trends in teaching and assessment methods in medical and dental education. J Educ Eval Health Prof [Internet]. 2021;18:13. Available from: http://dx.doi.org/10.3352/jeehp.2021.18.13
- Haleem , Javaid M., Qadri M. A., Suman R. Understanding the role of digital technologies in education: A review. Sustainable Operations and Computers [Internet]. 2022;3:275–85. Available from: http://dx.doi.org/10.1016/j.susoc.2022.05.004
- Kholoshyn , Nazarenko T., Bondarenko O., Hanchuk O., Varfolomyeyeva I. The application of geographic information systems in schools around the world: a retrospective analysis. J Phys Conf Ser [Internet]. 2021;1840(1):012017. Available from: http://dx.doi.org/10.1088/1742-6596/1840/1/012017
- Jeffries P. R., Bushardt R. L., DuBose-Morris R., Hood C., Kardong-Edgren , Pintz C. et al. The role of technology in health professions education during the COVID-19 pandemic. Acad Med [Internet]. 2022;97(3S):S104–9. Available from: http://dx.doi. org/10.1097/acm.0000000000004523
- Green N., Johnson C. D. Interprofessional collaboration in research, education, and clinical practice: working together for a better future. J Chiropr Educ [Internet]. 2015;29(1):1–10. Available from: http://dx.doi.org/10.7899/jce-14-36
- Darlow B., Coleman K., McKinlay E., Donovan S., Beckingsale L., Gray et al. The positive impact of interprofessional education: a controlled trial to evaluate a programme for health professional students. BMC Med Educ [Internet]. 2015;15(1). Available from: http://dx.doi.org/10.1186/s12909-015-0385-3
- Zechariah S., Ansa B. E., Johnson S. W., Gates A. M., Leo G. D. Interprofessional education and collaboration in healthcare: An exploratory study of the perspectives of medical students in the United States. Healthcare (Basel) [Internet]. 2019;7(4):117. Available from: http://dx.doi.org/10.3390/healthcare7040117
- Shawwa The use of telemedicine in medical education and patient care. Cureus [Internet]. 2023; Available from: http:// dx.doi.org/10.7759/cureus.37766
- Pit W., Velovski S., Cockrell K., Bailey J. A qualitative exploration of medical students’ placement experiences with telehealth during COVID-19 and recommendations to prepare our future medical workforce. BMC Med Educ [Internet]. 2021;21(1). Available from: http://dx.doi.org/10.1186/s12909-021-02719-3
- Macwilliam J., Hennessey I., Cleary G. Telemedicine: improving clinical care and medical education in Paediatr Child Health (Oxford) [Internet]. 2021;31(10):388–96. Available from: http://dx.doi.org/10.1016/j.paed.2021.07.004
- Civaner M. M., Uncu Y., Bulut F., Chalil E. G., Tatli A. Artificial intelligence in medical education: a cross-sectional needs BMC Med Educ [Internet]. 2022;22(1). Available from: http://dx.doi.org/10.1186/s12909-022-03852-3
- Nagi F., Salih R., Alzubaidi M., Shah H., Alam T., Shah Z. et al. Applications of artificial Intelligence (AI) in medical education: A scoping review. In: Studies in Health Technology and Informatics. IOS Press;
- Weidener L., Fischer M. Proposing a principle-based approach for teaching AI ethics in medical education. JMIR Med Educ [Internet]. 2024;10:e55368. Available from: http://dx.doi.org/10.2196/55368
- Forouzadeh , Kiani M., Bazmi S. Professionalism and its role in the formation of medical professional identity. Med J Islam Repub Iran [Internet]. 2018;765–8. Available from: http://dx.doi. org/10.14196/mjiri.32.130
- Andersson H., Svensson A., Frank C., Rantala A., Holmberg M., Bremer Ethics education to support ethical competence learning in healthcare: an integrative systematic review. BMC Med Ethics [Internet]. 2022;23(1). Available from: http://dx.doi. org/10.1186/s12910-022-00766-z
- Kanter S. L. Global health is more important in a smaller world. Acad Med [Internet]. 2008;83(2):115–6. Available from: http:// doi.org/10.1097/01.acm.0000305155.66318.58
- Jacobsen K. H., Waggett C. E. Global health education for the post-pandemic years: parity, people, planet, priorities, and Glob Health Res Policy [Internet]. 2022;7(1). Available from: http://dx.doi.org/10.1186/s41256-021-00234-y
- Drain K., Primack A., Hunt D. D., Fawzi W. W., Holmes K. K., Gardner Global health in medical education: A call for more training and opportunities. Acad Med [Internet]. 2007;82(3):226–30. Available from: http://dx.doi.org/10.1097/acm.0b013e3180305cf9
- Cordeiro Rodrigues L., Izugbara C., Carman M., van Dyk G. A. J., Umar E. Cultural competence must not leave anyone behind. Nat Hum Behav [Internet]. 2023;7(12):2040–1. Available from: http:// doi.org/10.1038/s41562-023-01739-x
- Dyrbye L. N., Shanafelt T. D., Gill P. R., Satele D. V., West C. P. Effect of a professional coaching intervention on the well-being and distress of physicians: A pilot randomized clinical trial. JAMA Intern Med [Internet]. 2019;179(10):1406. Available from: http:// doi.org/10.1001/jamainternmed.2019.2425
Information about the authors:
Boieva S. S. — Candidate of Medical Sciences, Lithuanian University of Helth Sciences, Kaunas, Lithuania.
Phone number: +38 (050) 732 17 32
ORCID: 0000-0002-2691-1895
Raksha-Slyusareva О. A. — Doctor of Medical Sciences, Full Professor, Professor at the Department of Microbiology, Virology, Immunology and Medical biology, Donetsk National Medical University, Lyman, Ukraine.
Phone number: +38 (095) 526 62 07
ORCID: 0000-0003-2144-6792
Slyusarev O. A. — Candidate of Medical Sciences, Docent, Head of the Department of Microbiology, Virology, Immunology and Medical biology, Donetsk National Medical University, Lyman, Ukraine.
Phone number: +38 (095) 495 32 15
ORCID: 0000-0002-2968-9388
Kovalenko Р. G. — Doctor of philosophy in Biology, Assistant of the Department at the Microbiology, Virology, Immunology and Medical biology, Donetsk National Medical University, Lyman, Ukraine.
Phone number: +38 (066) 321 29 76
ORCID: 0000-0003-4731-6902
Відомості про авторів:
Боєва С. С. — к. м. н., Литовський університет наук про здоров’я, м. Каунас, Литва.
Номер телефону: +38 (050) 732 17 32
ORCID: 0000-0002-2691-1895
Ракша-Слюсарева О. А. — д. м. н., професор, професор кафедри мікробіології, вірусології, імунології та медичної біології Донецького національного медичного університету, м. Лиман, Україна.
Номер телефону: +38 (095) 526 62 07
ORCID: 0000-0003-2144-6792
Слюсарев О. А. — к. м. н., доцент, завідувач кафедри мікробіології, вірусології, імунології та медичної біології Донецького національного медичного університету, м. Лиман, Україна.
Номер телефону: +38 (095) 495 32 15
ORCID: 0000-0002-2968-9388
Коваленко П. Г. — д. б. н., асистент кафедри мікробіології, вірусології, імунології та медичної біології Донецького національного медичного університету, м. Лиман, Україна.
Номер телефону: +38 (066) 321 29 76
ORCID: 0000-0003-4731-6902